By Asmau Ahmad
The Coordinating Minister of Health and Social Welfare, Professor Muhammad Ali Pate said the high cost of treatment creates a barrier to accessing hepatitis services in the African region.
He said this on Tuesday in Abuja at the 2023 African Hepatitis Summit with the theme ‘Putting Africa on track towards Viral Hepatitis Elimination.’
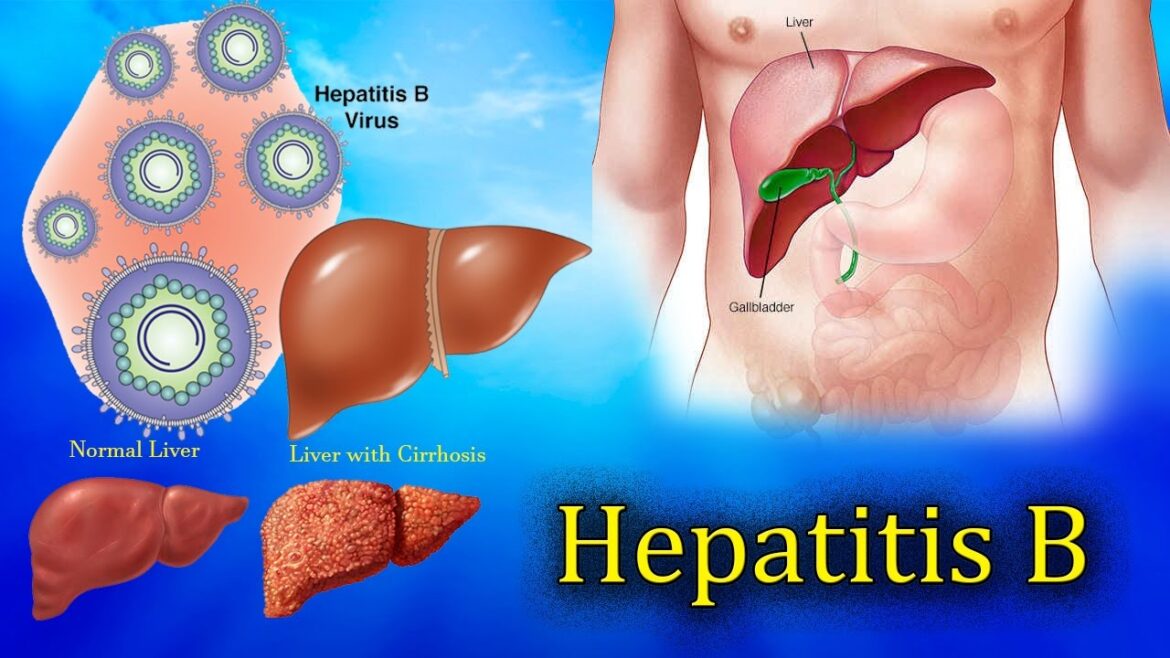
Prof. Pate said hepatitis continues to pose a huge public health threat, unleashing devastating consequences among patients grappling with chronic infections worldwide.
He, however, noted that hepatitis is preventable and curable, by putting in place a simplified approach deliverable at the primary level of care.
“This approach fortifies our ongoing and sustained commitment towards achieving universal health coverage by 2023. Currently, Africa battles with a substantial hepatitis burden, with 82 million and 9 million people living with Chronic Hepatitis B and Chronic Hepatitis C infections respectively.
“These staggering figures are further exacerbated by the fact that only 0.1 per cent of two per cent diagnosed with CHB and 0 per cent of 5 per cent diagnosed with CHC received treatment in the year 2020.
“These figures sharply contrast with the notable progress made globally, with 10 per cent of 296 million people diagnosed with CHB and 25 per cent of 58 million diagnosed with CHC receiving treatment, respectively,” he disclosed.
He said despite a 90 per cent risk of children acquiring CHB from mother-to-child transmission, only 14 out of 47 African countries have introduced routine hepatitis birth dose vaccination, and merely 17 per cent of newborns in Africa have received a timely hepatitis birth dose vaccination despite it being recognised as a cost-effective tool to prevent new infections.
“Indeed, it is high time African nations intensify efforts to increase immunization coverage. With the availability of affordable Directly Acting Anti-viral drugs for curing HCV and Tenofovir for treating HBV, African countries are strategically poised to overcome barriers to treatment, however, the high cost of treatment which is often paid out-of-pocket continues to create a barrier to access. It is high time African Nations collaborate to advocate for local production. We must also explore that health insurance is optimised.
“As we advocate for augmented financial commitment and support for hepatitis control response, it is imperative for African countries to align with the WHO’s new global health sector strategy, which has delineated new actions and targets to eliminate viral hepatitis by 2030. This strategy aims to curtail new infections and deaths to half a million each, globally – a reduction of 90 per cent and 65 per cent, respectively.
“Moreover, the need to sustain public awareness and build the capacity of healthcare providers is critical and plays a significant role in addressing knowledge gaps on hepatitis. We must ensure that those at risk of hepatitis are knowledgeable about the modes of transmission, how to prevent infection, and receive the care they need based on the principles of fundamental human rights, equity, and universal access to treatment using a primary healthcare approach,” he said.
Pate added that Nigeria is committed to achieving control of hepatitis towards elimination through the continuous strengthening of the primary healthcare system; public awareness campaigns; inclusion of hepatitis in the minimum package for national health insurance; capacity building of healthcare providers, integration into the HIV programme; strengthening birth dose routine immunisation, and collaboration with stakeholders to decentralise diagnosis and treatment of hepatitis.